Understanding Hypermobility
Article by Anna Kania
While some individuals may naturally possess hypermobile joints without adverse effects, others may experience symptoms that require attention.

What is Mobility?
Mobility refers to the ability of a joint to move through its full range of motion efficiently and without pain. Optimal mobility is essential for performing daily activities and maintaining overall musculoskeletal health.

What is Hypermobility?
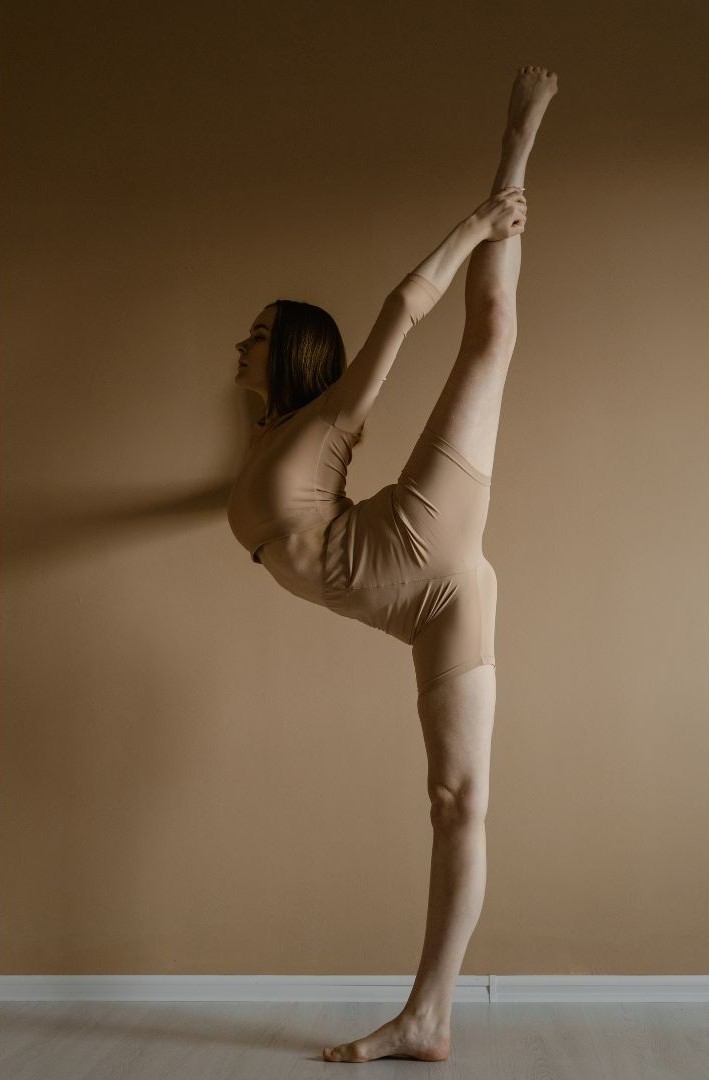
Hypermobility occurs when joints can move beyond the typical range expected for a particular joint. This increased flexibility is often due to variations in connective tissue components, such as collagen, which provides strength and elasticity to ligaments and tendons. While some individuals may naturally possess hypermobile joints without adverse effects, others may experience symptoms that require attention.
Signs of Hypermobility
Common indicators include:
- Joints that easily move beyond the normal range.
- Frequent joint dislocations or subluxations.
- Joint pain or stiffness, especially after physical activity.
- Clicking or popping sounds in joints.
- Fatigue or muscle pain.

Affected Joints
Hypermobility can impact various joints, including:
- Knees
- Elbows
- Shoulders
- Fingers
- Hips
- Spine
Comorbidities
Hypermobility may be associated with several conditions, such as:
- Ehlers-Danlos Syndrome (EDS): A group of connective tissue disorders characterized by hypermobile joints, skin hyperextensibility, and tissue fragility.
- Marfan Syndrome: A genetic disorder affecting connective tissue, leading to features like long limbs, flexible joints, and cardiovascular issues.
- Osteogenesis Imperfecta: A condition causing brittle bones, often accompanied by joint hypermobility.
- Fibromyalgia: A disorder characterized by widespread musculoskeletal pain, which may coexist with hypermobility.
- Chronic Fatigue Syndrome: Persistent fatigue that is not alleviated by rest and may be linked to hypermobility.
Risk of Being Hypermobile
While many individuals with hypermobility remain asymptomatic, potential risks include:
- Increased susceptibility to joint injuries, such as sprains or dislocations.
- Early-onset osteoarthritis due to increased wear on joint surfaces.
- Chronic joint or muscle pain.
- Development of conditions like scoliosis (curvature of the spine).
Management and Treatment
Not all cases of hypermobility require intervention. However, if symptoms are present, management strategies may include:
- Physiotherapy: A physiotherapist can design a personalized exercise program focusing on strengthening muscles around hypermobile joints, enhancing stability, and improving proprioception (awareness of joint position).
- Lifestyle Modifications: Avoiding activities that place excessive strain on hypermobile joints, maintaining a healthy weight to reduce joint stress, and using supportive footwear can be beneficial.
- Pain Management: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may help alleviate discomfort.
- Assistive Devices: In some cases, braces or supports may be recommended to stabilize affected joints during activities.
When to Seek Professional Advice
If you experience joint symptoms or are uncertain about your joint health, consider consulting a physiotherapist for an assessment. Early evaluation can aid in preventing potential complications and enhance quality of life. Additionally, if you experience systemic symptoms like dizziness, digestive issues, or unexplained fatigue alongside hypermobility, it is advisable to consult a general practitioner for a comprehensive evaluation.
Understanding hypermobility and its implications is crucial for effective management and maintaining joint health. With appropriate strategies, individuals with hypermobility can lead active and fulfilling lives.
References:
- Cleveland Clinic. “Joint Hypermobility Syndrome.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/21763-joint-hypermobility-syndrome. Accessed 31 Dec. 2024.
- Genetics Home Reference. “Ehlers-Danlos Syndrome.” MedlinePlus, U.S. National Library of Medicine, https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/. Accessed 31 Dec. 2024.
- Castori, Marco. “Ehlers-Danlos Syndrome(s) and Joint Hypermobility: The Need for Correct Diagnosis and Appropriate Care.” Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders, vol. 6, 2013, pp. 55–67. DOI: 10.4137/CMAMD.S12709. Accessed 31 Dec. 2024.
- Genetics Home Reference. “Marfan Syndrome.” MedlinePlus, U.S. National Library of Medicine, https://medlineplus.gov/genetics/condition/marfan-syndrome/. Accessed 31 Dec. 2024.
- U.S. National Library of Medicine. “Fibromyalgia.” MedlinePlus, https://medlineplus.gov/fibromyalgia.html. Accessed 31 Dec. 2024.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. “Joint Health and Hypermobility.” NIAMS, https://www.niams.nih.gov/health-topics/joint-problems-and-hypermobility. Accessed 31 Dec. 2024.
You May Also Like...
-
 ArticleView Post
ArticleView PostAre You Sitting Too Much?
Shocking statistics show globally 1 in 4 adults are not getting enough exercise. Let’s take a look at how E.A.S.Y. getting active can be!
-
 ArticleView Post
ArticleView PostRunning Without Injury: Risk Factors & Injury Management
Understand the risk factors associated with running and you’ll be able to hit the ground running while staying injury-free!
-
 ArticleView Post
ArticleView PostExercising during Pregnancy part 1 of 2: General Guidelines
A physically active pregnancy provides numerous health benefits for both mother and baby.